Rothmund-Thomson Syndrome (RTS)
Rothmund-Thomson syndrome, or RTS, is a rare disorder that is a member of a large group of conditions called ectodermal dysplasias (EDs) The EDs affect the development or function of several parts of the body: the teeth, hair, nails and sweat glands. Another ED in our database is Ellis-van Creveld syndrome. Trichothiodystrophy is also related to this group.
People with EDs may have sparse/thin hair or hair loss. They may also have dental abnormalities, including abnormally shaped teeth, very small teeth, abnormal roots, and missing teeth. Their fingernails may not form properly, and may be thin and split easily. Alternatively, their nails may be very thick. ED patients may develop rashes on their skin and have trouble sweating. Other features of EDs include large or prominent foreheads, chin abnormalities, and cataracts. For general information about EDs and a list of specific conditions, please visit the site of the Ectodermal Dysplasia Society (link in the column at the right).
The EDs are generally very rare diseases. Although RTS has been reported in people from many different races and ethnicities, it is very rare. The total number of cases reported in the literature is in the low hundreds (300 in 2010; 1).
Clinical information
The hair, nail, and dental abnormalities noted above are common in RTS, as are other problems including cataracts. In addition, people with RTS are at higher risk for cancer --- especially a form of bone cancer called osteosarcoma, which has been found in 40 out of 300 patients described in the literature (2). The most common clinical features of this syndrome are listed below.
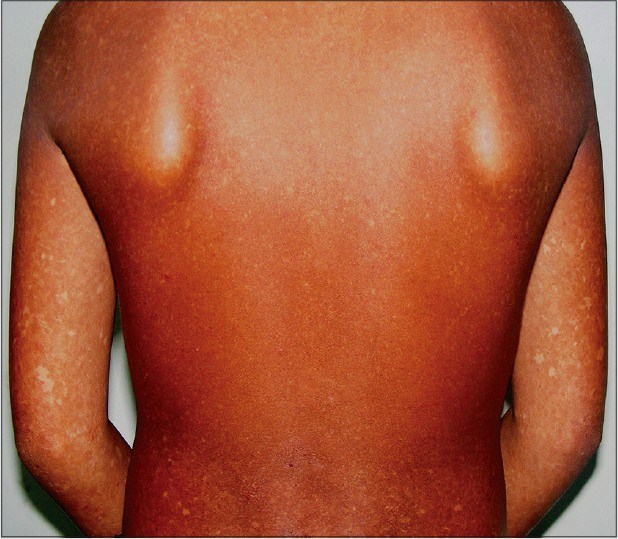
- Poikiloderma (a rash-type condition that usually begins on the face; see photos)
- Skin hyperkeratosis in areas (thickened, warty outer skin layer; see photo)
- Skin telangiectasias (spidery veins visible near the surface of the skin)
- Skin atrophy in areas affected by the rash
- Dental abnormalities (small teeth, etc.)
- Skeletal abnormalities (see photos)
- Baldness or patchy baldness
- Sparse or absent eyelashes
- Sparse or absent eyebrows
- Very short stature
- Abnormal nails
- Small hands
Common clinical features of RTS
Some people with RTS have radial ray defects. This term refers to underdevelopment of the radius bone in the arm (see photo at right). Radial ray defects can also affect the thumb, which may be small, malformed, or completely absent. The x-ray at the right shows a person who was missing a thumb and wrist bones.
Most people with RTS have normal intelligence (1). For example in our literature survey, we found that intelligence was normal in 90% of patients.
There are two forms of RTS, called type 1 and type 2. Members of both groups have poikiloderma. Type 1 RTS is also characterized by cataracts, and ectodermal dysplasia. Patients with type 2 RTS have congenital bone defects such as thumb and arm malformations and/or other problems, and an increased risk of osteosarcoma.
Roughly two-thirds of all tested RTS cases have mutations in a gene called RECQL4 (3; reviewed in 1). In addition, mutations that cause of loss of this gene are associated with an increased risk for osteosarcoma (4).
RTS is an autosomal recessive disorder caused by mutations in the gene RECQL4. The term autosomal recessive means that the syndrome occurs when both parents carry a mutated copy of a gene, and each passes the mutated copy to a child. Each parent will have one copy of the gene with the mutation and one copy of the gene without the mutation. This means that there is a one chance in four that future children will also have RTS.
Two other conditions are caused by mutations in RECQL4 They are Baller-Gerold syndrome (BGS) and a condition named RAPADILINO syndrome. Both conditions involve abnormal bone development. BGS is characterized by radial ray defects, other skeletal abnormalities, and short stature, all of which occur in RTS. BGS patients also have craniosynostosis, or premature fusion of the skull bones. This feature is rare in people with RTS. People with RAPADILINO syndrome also have radial ray defects as well as undeveloped or absent kneecaps (a problem that also occurs in RTS). They have short stature and may develop café-au-lait spots, but no poikiloderma. Gastrointestinal problems also occur. The letters in the name RAPADILINO stand for the following terms: RA: radial ray malformations; PA: patella and palate abnormalities; DI: diarrhea and dislocated joints; LI: limb abnormalities and little size; and NO: slender nose and normal intelligence.
Diagnosis and Testing
The diagnosis of RTS is based on clinical observations and testing. According to the National Institutes of Health (5), diagnosis is according to the criteria described below.
A definite diagnosis can be made if poikiloderma has a pattern as follows: the rash starts in infancy (usually between age 3-6 months). At first, it looks like redness/erythema on the cheeks and face. Next, it spreads to the extensor surfaces of the extremities. The trunk and abdomen are not usually affected, though the buttocks may be involved. This phase is called the acute phase. Over a period that lasts for months or years, pigment in the skin affected by the rash is altered, and telangiectases and atrophy atrophy appear. This condition is called the chronic phase and the changes are permanent.
A possible diagnosis can be made in a person with 1) a rash that does not fit the pattern above because of how it looks, how it is distributed on the body, or how and when it begins and spreads, and 2) two of the following clinical features:
- Sparse scalp hair, eyelashes, and/or eyebrows
- Small size that is symmetrical in the body
- Gastrointestinal problems in young children that may require a feeding tube (e.g. vomiting or diarrhea)
- Radial ray defects
- Skeletal abnormalities (dysplasias, absent or malformed bones, osteopenia, abnormal trabeculation)
- Dental abnormalities (rudimentary or poorly formed teeth, enamel defects, delayed tooth eruption, small roots)
- Hyperkeratosis, especially on the soles of the feet
- Cataracts in both eyes, typically before adulthood
- Osteosarcoma or other cancers, such as skin cancers
Common clinical features of RTS
Laboratory testing may also identify mutations in the gene RECQL4. Abnormalities of chromosome 8 have also been found (RECQL4 is on chromosome 8). They include trisomy (three copies of the chromosome), duplications of a part of the chromosome called 8q, and tetrasomy four copies) of 8q. Mutations and chromosomal abnormalities are not found in every person with RTS (1).
Differential Diagnosis
A number of rare conditions can resemble RTS. They are listed below.
Xeroderma pigmentosum (XP). XP is a rare disorder that causes extreme sensitivity to ultraviolet/UV light. Many people with XP can be severely sunburned after spending only a few minutes in sunlight, with some even burning if they stay in the shade. Some people with XP do not burn easily, but the sensitivity to UV light is still present, and is still very dangerous. The danger exists because XP patients are unable to repair the damage that UV light does to DNA. The result is that they are highly susceptible to skin cancer, with a risk that is ~10,000 times the risk for unaffected people (reviewed in 6). In practice, this means that XP patients may develop skin cancers at young ages, with many developing cancers before age 8. Cancer incidence can be greatly reduced by strict protection from UV light. People with XP generally do not have the skeletal abnormalities that are common in RTS. Lesions on their eyes and scalp may cause eyelashes and hair loss, but people with XP do not typically suffer from generalized hair loss like RTS patients. Dental problems such as very small teeth and small roots are not features of XP, but are common in RTS.
XP does not cause the skeletal abnormalities that are common in RTS. Additionally, although lesions on and near their eyes may cause them to lose eyelashes, this problem does not tend to happen in the absence of lesions, and XPers do not generally suffer from hair loss like RTS patients. Dental problems such as very small teeth and small roots are not features of XP, but are common in RTS.
XP-neurological disease. XP-Neuro is a form of XP that adds neurological problems to the skin and other problems in XP. People with XP-Neuro may have additional clinical features that are common in RTS, such as very short stature, microcephaly, and intellectual disability. Like XP, however, XP-Neuro patients do not generally have skeletal abnormalities or hair eyelash loss unless it is due to lesions. Neurological problems in XP-Neuro may be show as early as toddlerhood, but they may not become apparent until adulthood (6). The neurological problems in XP-Neuro are progressive, meaning that they get worse with time. This is not the case in RTS.
People with XP tend to develop skin lesions on sun-exposed areas, with protected areas being spared, while RTS patients develop skin lesions on sun-protected areas. The sun may make lesions worse in both groups, but an important difference is that the presence of skin lesions in protected areas is more characteristic of RTS.
Cockayne syndrome (CS). CS, like XP, is a very rare disorder that causes sensitivity to ultraviolet/UV light. Many people with CS can be severely sunburned after brief exposures to the sun, though some can spend time outside when using sunscreen. Unlike XP, CS does not increase cancer risk. In fact, cancer does not generally occur in people with CS. CS patients do not develop the skin lesions that are characteristic of XP (7). Note that people with an extremely rare condition called XP-CS complex are susceptible to cancer (see below).
As is the case with XP-Neuro, the neurological problems in CS are progressive, meaning that they get worse with time. This is not the case in RTS. Intellectual disability is almost universal in CS, and it is uncommon in RTS. CS patients also develop a recognizable facial appearance that is very different from that of people with RTS.
XP-CS complex (XP-CS) is a combination of xeroderma pigmentosum and Cockayne syndrome. The clinical features described for each of these conditions occur in XP-CS: sensitivity to ultraviolet/UV light, the development of lesions on sun-exposed skin, very short stature, intellectual disabilities, and a predisposition to cancer (especially skin cancer). As with XP-Neuro and CS, the neurological problems in XP-CS are progressive.
Werner syndrome (WS) is a rare genetic disease characterized by an appearance of premature aging combined with medical problems normally associated with older age. These problems generally begin to show around the time of adolescence, such as when a teenage growth spurt does not occur. WS's clinical features include cataracts, premature greying of the hair and hair loss, and skin changes called scleroderma, which make the skin hard and tight. Like RTS patients, WS patients have a high cancer risk (8). A key difference between the two syndromes is the age of onset: the clinical features of RTS generally appear by age 2, while the features of WS do not appear until adolescence. People with WS often develop type 2 diabetes, as well, a problem that is not generally associated with RTS. WS is more common in people of Japanese and Sardinian descent.
Bloom's syndrome (BSyn) is a rare condition that shares many similarities with RTS. For example, BSyn patients are generally very small from the time of birth and are sensitive to light. They also develop a facial rash with telangiectasias and blistering, and develops on sun-exposed skin. Although this rash is described as "not a true poikiloderma" (5), it can look similar to the rash in RTS. Patients may also develop café-au-lait spots, which are areas of too much skin pigment. They occur on areas of their skin that are not exposed to light. Areas of too little skin pigment also occur. Other clinical features that are shared with RTS include frequent infections and a high cancer risk, including osteosarcoma (9). Features that may help distinguish the two diseases include a high-pitched voice that is characteristic of Bloom syndrome, but not RTS. Bloom patients may also have extra fingers and cysts at the bases of their spines. In the laboratory, Bloom syndrome may be identified by testing for increased sister chromatid exchanges (SCEs) in cells exposed to a substanced called bromodeoxyuridine. Bloom syndrome is the only known condition in which SCEs increase under these circumstances (5).
Other conditions related to RTS are described in references 1 and 5.
References
- 1. Larizza L et al. (2010) Rothmund-Thomson syndrome. Orphanet J Rare Dis 5:2. doi: 10.1186/1750-1172-5-2. Full text on PubMed.
- 2. Zils K et al. (2015) Osteosarcoma in patients with Rothmund-Thomson syndrome. Pediatr Hematol Oncol 32(1):32-40. Abstract on PubMed.
- 3. Kitao S et al. (1999) Mutations in RECQL4 cause a subset of cases of Rothmund-Thomson syndrome. Nat Genet 22(1):82-84. Abstract on PubMed.
- 4. Wang LL et al. (2003) Association between osteosarcoma and deleterious mutations in the RECQL4 gene in Rothmund-Thomson syndrome. J Natl Cancer Inst 95(9):669-674. Full text from publisher.
- 5. Wang LL & Plon SE (1999) Rothmund-Thomson Syndrome. Updated January 3, 2019. GeneReviews [Internet] Pagon RA et al., editors. Seattle (WA): University of Washington, Seattle; 1993-2021. Full text.
- 6. Lehmann AR et al. (2011) Xeroderma pigmentosum Orphanet J Rare Dis 6:70. doi: 10.1186/1750-1172-6-70. Full text on PubMed.
- 7. Natale V (2011) A comprehensive description of severity groups in Cockayne syndrome. Am J Med Genet Part A 155A(5):1081-1095. Full text from Forgotten Diseases.
- 8. Oshima J et al. (2002) Werner Syndrome. Updated March 27, 2014. GeneReviews [Internet] Pagon RA et al., editors. Seattle (WA): University of Washington, Seattle; 1993-2021. Full text.
- 9. Calvert GT et al. (2012) At-risk populations for osteosarcoma: the syndromes and beyond. Sarcoma 2012:152382. doi: 10.1155/2012/152382. Full text on PubMed.
- 10. Guerrero-González GA et al. (2014) Rothmund-thomson syndrome: a 13-year follow-up. Case Rep Dermatol 6(2):176-179. Full text on PubMed.
- 11. Photo by Hellerhoff and found on the Wikimedia Commons..
- 12. Bartyik K et al. (2013) Rothmund-thomson syndrome and cutan T-cell lymphoma in childhood. Open J Pediatr 3:270-27. Full text.
- 13. Mahajan VK et al. (2015) Rothmund-Thomson syndrome with bronchiectasis: an uncommon phenotype? Open J Pediatr 81(2):190-192. Full text from publisher.
- 14. Popadić S et al. (2006) Rothmund-Thomson syndrome. The first case with plantar keratoderma and the second with coeliac disease. Acta Dermatovenerol Alp Pannonica Adriat 15(2):90-93. Full text from publisher.