Cockayne syndrome (CS)
CS is a member of a group of diseases called DNA repair disorders. These disorders cause problems with fixing damaged DNA. Damage to DNA happens constantly. It is caused by such things as ultraviolet light in sunlight and flourescent lights. Other things that can damage DNA include ionizing radiation from X-rays and other medical devices. Chemicals, normal processes in cells, and other substances or processes can also damage DNA. Because damage occurs all the time, living things have evolved many systems for fixing it. There are proteins that recognize that damage has occured, enzymes that remove the damaged DNA, and enzymes that insert new, undamaged DNA bases. This list is not exhaustive. When a person has a defect in one of these repair systems, disease results. If the problem is in a system that fixes damage from UV light, a person may be extremely photosensitive, with some people burning badly after only a brief exposure on a cloudy day. Overall, DNA most people with DNA repair disorders have a high risk of cancer. CS is an exception to this rule --- CS patients do not have an increased cancer risk. In fact, they do not generally get cancer. The reason for this is not understood.
CS is a member of a DNA repair disorder subgroup in which repair of UV-induced damage is defective. CS patients can be very prone to sunburn as a result, although not all patients have this problem. They also have a variety of medical problems that affect many systems in their bodies. CS is a progressive disorder, which means that it gets worse with time. Unlike most patients with UV-DNA repair disorders, most CS patients are not at increased risk of cancer. This fact may be due to the severity of CS.
Clinical information
Cockayne syndrome is an extremely rare disorder that affects many body systems. Its incidence in four countries in Western Europe (France, Italy, UK, Netherlands) is estimated at 2.7 per million births in the overall population, and 1.8 per million births among indigenous Europeans (1). In Japan, incidence is 2.8 per million births (Kubota). Estimates have not been made for other countries, but the figures are likely the same, with the exception of individual areas and groups where incidence is higher (e.g., among certain aboriginal Canadians and in Saudi Arabia).
CS is present at birth, although it may not be fully evident until 1-2 years of age in mildly affected patients. In many moderate or mild patients, the first sign of the syndrome may be photosensitivity (ranging from mild to severe), or unusually tight joints caregivers may notice that the hips are stiff when changing diapers). Severely affected patients may be born with cataracts and other medical problems that make the presence of the syndrome more obvious. Feeding difficulties are also very common in CS patients, although these problems tend to be less severe in very mild cases of the disease. In severely affected patients, tube feeding has been credited by many parents as extending life. CS patients commonly have the following problems:
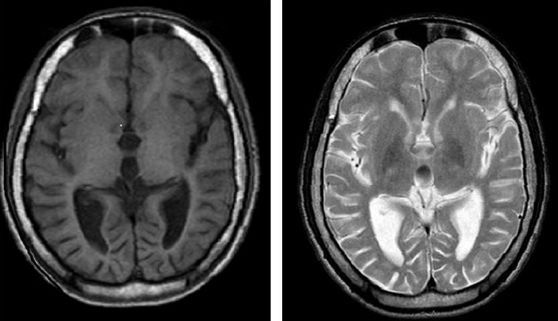
- Brain abnormalities on CT or MRI scans (calcifications, white matter abnormalities, atrophy)
- Gait ataxia (a stiff, unbalanced gait) in those who can walk; nay walk on toes
- Intellectual disability (ranges from mild to profound)
- Delayed development of fine and gross motor skills
- Hearing loss, which can happen suddenly
- Pigmentary abnormalities in the retina
- Photosensitivity (easy sunburning)
- Abnormal curvature of the spine
- Microcephaly (very small head)
- Very short stature/dwarfism
- Many dental cavities
- Peripheral cyanosis
- High blood pressure
- A distinctive voice
- Joint contractures
- Hand tremors
- A happy, gentle, and/or outgoing personality
Common problems in CS
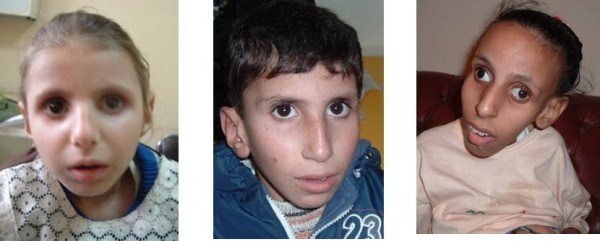
People with CS tend to have a similar facial appearance (see photos). The list below has features are often observed in this group. Note that some features may not be obvious in more mildly affected patients.
- Beaked nose (nose may have a bump that resemble a bird's beak)
- Receding jaw; typically in severely affected patients)
- Deep-set/sunken eyes (see photos on this page)
- Maloccluded/crowded teeth
- Small jaw
- Large ears
Common facial features in CS
Severity groups
There are four primary severity groups in CS: severe, moderate, mild, and adult-onset. The syndrome may be thought of as occuring on a continuous scale, although most patients can be classified into a severity group relatively easily. In severely affected patients, the presence of a congenital disorder is generally present at birth. Severely affected CS patients are smaller: in a recent survey, the average height at age 6 years in severely affected patients was 79 cm, or 31", with a range of 75 - 87 cm (3). These children achieve relatively few milestones, and have very short life expectancy. They typically do not learn how to walk independently, with the most severely affected children also not developing an ability to sit independently. Severely affected children tend to have no speech or <10 words, although many be able to communicate to varying degrees via sign language.
Some patients with the severe form of CS have been diagnosed as having Cerebro-ocular facial syndrome (COFS). Many patients with COFS have mutations in the CSB gene (reviewed in reference 3), and COFS appears to be a very severe form of CS.
Feeding difficulties and failure to thrive are universal or near-universal in this group, with cachexia being a significant problem. Children with severe CS typically need feeding tubes. Parents note that the tubes can help with weight gain and ease the administration of medicines and vitamins (personal communications to the author of this article). It is important to note that children with severe CS are prone to weight loss in the event of gastrointestinal infections. Any CS patient with such an infection should be seen by a doctor quickly and monitored closely.
Moderately affected CS patients tend to live longer and be bigger than children in the severe group. For example, the average height at age 6 in the study referenced above was 99 cm (39"), with a range of 91 - 107 cm (3). At age 16, these patients averaged 104 cm (~41"), with a range of 91-107 cm. In general, members of this group also achieve more milestones, with independent walking and self-feeding being common in this group. Coginitively, moderately affected patients typically learn to speak, although a minority may not. Some moderately affected patients acquire enough language to combine words/speak in phrases.
Feeding difficulties and failure to thrive are also very common in this group, with cachexia also being a significant problem. Many moderately affected children eat by mouth for many years. Soft foods such as yoghurts are the easiest for them to eat, while foods with mixed textures (e.g. crunchy cereal in milk) may be problematic. Many of these children benefit from feeding tubes, which offer the advantages noted in the previous paragraph. As with severe CS, it is important to note that moderately affected children are prone to weight loss in the event of gastrointestinal infections. Any CS patient with such an infection should be seen by a doctor quickly and monitored closely.
Those with the mild form of CS tend to be larger than those in the moderate group. Average height at age 6 in the study noted above was 104 cm (~41"), with heights at age 16 averaging 128 cm (50.4"; range: 107 - 148 cm; 3). In addition to being larger, these individuals may not have failure to thrive, may learn to speak in sentences and may learn to read, write, swim, ski, or ride a bike. These patients have the longest life expectancy.
The adult-onset form of CS has only been documented in a single case in Japan (4).
The table below shows average life expectancy for the severe, moderate, and mold forms of CS.
Mean life expectancy |
Range | ||
Severe |
5.1 years |
0.6 - 11 years |
|
Moderate |
15.9 years |
11 - 22 years |
|
Mild |
30.6 years |
22 - 47 years |
CS is a progressive disorder, which means that it gets worse with time. Regardless of severity group, the course of the disease is the same in all affected individuals. Patients initially grow and gain skills, plateau, and then go through a period of decline during which skills are lost and medical problems increase. The length of each stage is correlated with severity. Growth and skill acquisition are shortest in the most severely affected, and longest in the most mildly affected, while skill loss is the most rapid in severe CS and slowest in mildly affected patients. Anxiety may develop as a result of skill loss. Hearing loss is a particularly common reason for the development of this problem. Cochlear implants have been transformative for some patients in that regard (3, 5).
Dysphagia (swallowing difficulties) can be a significant problem in declining CS patients. This problem can lead to aspiration of food, airway blockage, or aspiration pneumonia. It may be advisable to avoid firm chokable foods such as apples, etc. in patients with dysphagia. Soft foods such as yoghurts may be more easily tolerated, and feeding tubes may also be recommended by physicians.
CS has been described as involving post-natal growth failure, with prenatal growth in children in the moderate and mild groups being normal, and growth faltering after birth (6).
Diagnosis, Testing, and Clinical Trials
CS is confirmed by testing for mutations in the genes CSA/ERCC8 and CSB/ERCC6, and for XP-CS (see below), XPB, and XPD. The US National Institutes of Health maintains a list of laboratories that do testing (see link at right). If you are not a doctor and suspect that your child has CS, check with your family physician, who will compare your child's signs and symptoms with those known to occur in this syndrome. If your child's doctor isn't familiar with CS, the information sources on this page may help. Your doctor can obtain a sample from your child and send it to a testing center.
Since 1999, the National Institutes of Health has been running a large study of people with TTD, Cockayne syndrome, and xeroderma pigmentosum. The study is called Examination of Clinical and Laboratory Abnormalities in Patients with Defective DNA Repair: Xeroderma Pigmentosum, Cockayne Syndrome, or Trichothiodystrophy. The goal of the study is to document health problems occuring in people with these diseases in order to understand them as completely as possible. More information about the study, including contact information, is available at clinicaltrials.gov.
Differential Diagnosis
Xeroderma pigmentosum-Cockayne syndrome complex (XP-CS). In most ways, XP-CS is effectively the same disease as CS. The primary difference between the two is that XP-CS patients have the features of XP in addition to having CS. Having XP increases their cancer risk --- while CS patients do not appear to get cancer (9), XP-CS patients do. However, the risk in XP-CS appears to be lower than the risk among other XP patients (10). However, these patients do suffer from disfiguring skin changes caused by exposure to UV light, and therefore, XP-CS patients should be carefully protected from sunlight and other sources of UV light. Apart from factors related to the skin, strategies for managing XP-CS and CS are generally the same.
Trichothiodystrophy (TTD). TTD is another DNA repair disorder that is often mistaken for CS. People with TTD have short stature, intellectual disabilities, a small head (microcephaly), and white matter abnormalities on a brain scan. They may also have cataracts, feeding difficulties in infancy, failure to thrive, hearing loss, cavities, and dry eyes. All of these problems are common in CS. The main difference between the two diseases is that TTD patients have specific abnormalities of their hair and nails that CS patients don't have. Nails in TTD may be brittle and may split easily. Hair in TTD tends to be dry and very brittle hair, and it also may break easily. When a TTD hair sample is examined under a standard microscope, a small number of hairs will have breaks that look like the ends of paintbrushes. Hair from people with TTD also has a tiger-tail pattern when examined using a technique called polarizing microscopy. Our TTD page has photos for both of these abnormalities. Hair from CS patients does not have these problems. Like CS and many other conditions, the severity of TTD ranges from mild to severe. Severely affected patients may be as small as CS patients, while mildly affected patients may grow to be several inches taller.
References
- 1. Kleijer WJ et al. (2008) Incidence of DNA repair deficiency disorders in western Europe: Xeroderma pigmentosum, Cockayne syndrome and trichothiodystrophy. DNA Repair (Amst) 17(5):744-750. Abstract on PubMed.
- 2. Kubota M et al. (2015) Nationwide survey of Cockayne syndrome in Japan: Incidence, clinical course and prognosis. Pediatr Int 57(3):339-347. Abstract on PubMed.
- 3. Natale V (2011) A comprehensive description of severity groups in Cockayne syndrome. Am J Med Genet Part A 155A(5):1081-1095. Abstract on PubMed. Full text from Forgotten Diseases Research Foundation.
- 4. Hashimoto S et al. (2008) Adult-onset neurological degeneration in a patient with Cockayne syndrome and a null mutation in the CSB gene. J Invest Derm 128:1597-1599. Full text from publisher.
- 5. Morris DP et al. (2007) Cochlear implantation in Cockayne syndrome: our experience of two cases with different outcomes. Laryngoscope 117(5):939-43. Abstract on PubMed.
- 6. Laugel V (2000) Cockayne Syndrome Updated June 14, 2012. GeneReviews [Internet] Pagon RA et al., editors. Seattle (WA): University of Washington, Seattle; 1993-2021. Full text.
- 7. Oken E et al. (2003) A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr 3:6. doi:10.1186/1471-2431-3-6 Full text on PubMed.
- 8. Roberts CL et al. (1999) National birthweight percentiles by gestational age for twins born in Australia. J Paediatr Child Health 35(3):278-282. Abstract on PubMed.
- 9. Zhang WR et al. (2016) Absence of skin cancer in the DNA repair-deficient disease Cockayne Syndrome (CS): a survey study. J Am Acad Dermatol 74(6):1270-1272. Abstract on PubMed.
- 10. Natale V & Raquer H (2017) Xeroderma pigmentosum-Cockayne syndrome complex. Orphanet J Rare Dis 12(1):65. doi: 10.1186/s13023-017-0616-2. Full text on PubMed.
- 11. Batra PS et al. (2008) Infantile onset of Cockayne syndrome in two siblings. Indian J Dermatol Venereol Leprol 74(1):65-67. Full text from publisher.
- 12. Ghaffar TYA et al. (2011) Cholestasis in patients with Cockayne syndrome and suggested modified criteria for clinical diagnosis. Orphanet J Rare Dis 6:13. doi: 10.1186/1750-1172-6-13 Full text on PubMed.
- 13. Mundaganur P (2012) A rare case of Cockayne syndrome-MRI features. J Clin Diagn Res 6(9):1582-1583. Full text on PubMed.