Turner Syndrome (TS)
Turner syndrome (TS) affects females. It is caused when one of a girl's two X chromosomes is absent or damaged. TS is the most common chromosomal abnormality in females, and is therefore relatively common among the rare diseases. Studies from around the world estimate it as occurring in roughly 1 female infant in every 2,000 to 3,000 live female births (1-4). In addition, it is estimated to affect up to 3% of all female fetuses (5, 6), with death in the fetal period occuring at a high rate (7).
Clinical information
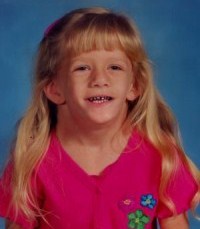
The signs of Turner syndrome may be evident before or at birth, but they may not appear until much later. For example, amniocentesis may show chromosomal abnormalities. Additionally, ultrasound findings may indicate TS. They include fluid collection around the neck, heart, or kidney abnormalities and/or poor growth, among other findings. At birth, signs of Turner include swelling of the hands and feet, along with webbing of the neck and/or extra skin folds around the neck. Girls with TS tend to be very short, and do not generally enter puberty at the normal age. Growth hormones can help normalize height.
Fertility problems are a major concern for women with TS (reviewed in 8). In many patients, there is poor or no development of the uterus. In addition, many girls with TS have streak ovaries. This term means that their ovaries are composed mainly of fibrous tissue that does not produce either hormones or eggs. These problems result in infertility. Treatment with hormones can alleviate the problem, but not resolve it. Patients tend to experience loss of ovarian function in childhood, although a small number may have normal menses until their mid-20s. Studies of spontaneous puberty (including menses) in TS have found it in as few as 5% of study subjects and as many as 20% (9). Spontaneous pregnancy has been reported in a small percentage of women with TS (9, 10).
Overall, very short stature and abnormalities of the reproductive system are the most common problems in TS. Many common clinical features of the syndrome are listed below.
- Very short stature (small size may or may not be evident at birth)
- Cubitus valgus deformity (forearm is abnormally angled away from the body)
- A broad chest with widely-spacedn nipples (a "shield chest)
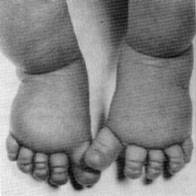
- Puffy hands and feet (often evident in infancy; see photo)
- Webbing around the neck (see photos on this page)
- Skin moles (may not appear until after age 4)
- Finger- or toenail abnormalities (see photo)
- Low hairline at the back of the head
- Underdeveloped or absent uterus
- Congenital kidney problems
- Congenital heart problems
- Delayed bone development
- Delayed or absent puberty
- Thyroid abnormalities
- Ear infections
- Hearing loss
Common clinical features of Turner syndrome
Most girls and women with TS do not have all of the problems listed here. As noted, the most common ones are short stature and underdevelopment of the uterus.
Puffiness of the hands and feet, known as lymphedema, occurs in a majority of newborns with Turner syndrome. Its presence in a newborn can facilitate early diagnosis, with expert opinion noting that "lymphedema in a female newborn should always suggest the diagnosis of Turner syndrome" (11).
Overall, intelligence is normal in most people with Turner syndrome, although a minority may have low IQs. Specific learning disabilities also occur, especially in the areas of math, visuospatial abilities, and executive function (reviewed in 8).
Girls and women with Turner syndrome share many characteristics of the face, head, and neck. For example, many have extra folds of skin around their necks at birth. Webbing at the neck may also be apparent at that time, or it may develop later (see photos on this page). Neck webbing develops because fluid collects in the back of the neck before birth. The fluid is the cause of extra skin folds that can develop a webbed appearance. The trait may be apparent on an ultrasound. Cosmetic surgery can remove it.
Other common features of head and neck in TS include a large forehead, low-set ears that may point toward the back of the head, a small jaw, a droopy eyelid (see photo at top right), strabismus (eyes are not aligned; may be crossed or point outward), and skin folds over the inner part of the eye. These folds are called epicanthal folds; they occur normally in people of east Asian descent.
Cause
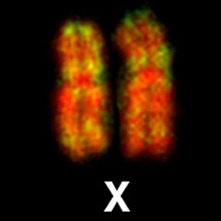
The cause of Turner syndrome was discovered in 1959 (12). TS is a chromosomal disorder involving the sex chromosomes. Humans have 46 chromosomes. Two determine sex. They are called X and Y chromosomes. Girls have 2 X chromosomes, and boys have 1 X and 1 Y chromosome. TS happens when there is complete or partial loss of one X chromosome. Girls with full loss of one X chromosome are described as 45,X, which means that they have 45 chromosomes instead of 46, and are missing 1 X chromosome.
Some girls have 46 chromosomes in some of their cells and 45 in others. This combination is called mosaicism, and patients are described as being 45,X/46X,Y. Patients in this group may have milder symptoms than those in the 45,X group. For example, they tend to be more likely to begin menstruating spontaneously and seem to be more likely to become pregnant without fertility treatment (13). Nonetheless, the rate of sponteneous pregnancy is very low in TS, even in this group (13).
Many other variations in X chromosome abnormalities can cause TS. Some of them are structural problems in the X chromosome, such as when an X chromosome abnormally forms a ring structure or when part of the chromosome is lost and is replaced by a duplicated existing piece.
Boys may also lose some or all of a sex chromosome. Depending on what has been lost, they may have some of the clinical features that are associated with Turner syndrome (described as Turner-like). However, because TS is defined as affecting girls, these boys do not have TS. These boys may have Noonan syndrome, which is similar to TS (see Differential Diagnosis, below).
Diagnosis and Testing
Because TS is a chromosomal disorder involving the X chromosome, definitive diagnosis depends on laboratory testing. In order to be diagnosed with TS, a female person must have a positive lab test clinical features of TS, such as short stature and/or defects of the ovaries, cardiovascular system, and kidneys (14). It is important to note again that while males may have clinical features shared with Turner syndrome, they are excluded from diagnosis, as the syndrome is defined as affecting females only.
A type of test called a chromosomal karyotype has been the standard laboratory test for TS for many decades. In recent years, however, newer, tests have entered development. These tests use genomic techniques, and they may simplify diagnosis in the future (14). Some are already in use (see the link for testing at right for examples).
American Family Physician has two excellent documents about Turner syndrome. The first contains information about testing and diagnosis. The second one concerns treatment and management of TS.
Differential Diagnosis
A small number of other conditions resemble Turner syndrome.
Noonan syndrome (NS). NS and TS share many clinical features. They include low-set ears that may point toward the back of the head, short webbed necks, excess skin around the neck in infancy, and droopy eyelids (ptosis). This list is not comprehensive. People with both syndromes may be born with cardiac abnormalities, and may also be short with wide chests, widely spaced nipples, and delayed bone age.
Chromosome testing can distinguish TS and NS. In addition, certain specific clinical features can also help. For example, heart defects in TS tend to occur on the left side of the heart, with bicuspid aortic valves and coarctation of the aorta being the most common. In NS, the most common problems are pulmonary valve stenosis (narrowing of the pulmonary artery) and hypertrophic cardiomyopathy (thickening of the heart, which can create problems with pumping blood).
46,XX gonadal dysgenesis. Women with this condition have primary amenorrhea. This term means that they do not begin menstruating by their 16th birthdays. This problem may lead to a suspicion of Turner syndrome. However, unlike TS patients, people with this condition do not have short stature or congenital heart defects. They also do not have facial and other features of TS, such as a webbed neck and other facial features. Laboratory karyotype testing in people with this disorder shows a normal female result (46,XX).
Swyer syndrome (46,XY gonadal dysgenesis) (SS). Individuals with this condition have typical female genitalia, but have male sex chromosomes (X,Y). As with 46,XX gonadal dysgenesis, people with SS have primary amenorrhea, which may lead to a suspicion of Turner syndrome. Unlike TS patients, Swyer syndrome patients are not short, and they do not generally have congenital heart defects. Testing reveals a 46X,Y karyotype. SS is associated with a number of genes (see list), including SRY. SRY is on the Y chromosome. It is responsible for initiating processes that are part of male sexual development. When it does not function properly, these processes cannot occur.
People with SS are usually raised as females. Their ovaries do not function, but hormone replacement therapy can help induce menstruation and the development of female physical characteristics, including breast development and growth of the uterus. They may be able to become pregnant through the use of donated eggs or embryos.
Hereditary lymphedema type IA (Milroy disease). This condition affects boys and girls. It is characterized by swelling, which is often (but not always) present at birth or soon afterward. This trait causes it to be mistaken for Turner syndrome or vice-versa. Although the location of the swelling varies considerably among individuals, the legs and feet are most often affected --- hence the similarity to TS. Unlike TS, Milroy disease may run in families. Other clinical features that can help distinguish it from TS include wart-like growths called papillomas and prominent veins in the legs. Boys may be born with a fluid-filled sac in the scrotum (a hydrocele). Milroy disease is associated with the gene FLT4. Patients have a normal karyotype.
Other conditions in the differential diagnosis of Turner syndrome are described in reference Lowenstein.
References
- 1. Adeyokunnu AA (1982) The incidence of Turner's syndrome in Ibadan, Nigeria. Afr J Med Med Sci 11(3):105-112. Abstract on Pubmed.
- 2. Nielsen J & Wohlert M (1991) Chromosome abnormalities found among 34,910 newborn children: results froma 13-year incidence study in Arhus, Denmark. Hum Genet 87(1):81-83. Abstract on Pubmed.
- 3. Gravholt CH et al. (1996) Prenatal and postnatal prevalence of Turner's syndrome: a registry study. BMJ 312(7022):16-21. Full text on Pubmed.
- 4. Stochholm K et al. (2006) Prevalence, incidence, diagnostic delay, and mortality in Turner syndrome. J Clin Endocrinol Metab 91(10):3897-3902. Full text on publisher's website.
- 5. Cockwell A et al. (1991) A cytogenetic and molecular study of a series of 45,X fetuses and their parents. J Med Genet 28(3):151-155. Full text on Pubmed.
- 6. Menasha J et al. (2007) Incidence and spectrum of chromosome abnormalities in spontaneous abortions: new insights from a 12-year study. Genet Med 7(4):251-263. Abstract on PubMed. Full text on publisher's website.
- 7. Hook EB & Warburton D (1983) The distribution of chromosomal genotypes associated with Turner's syndrome: livebirth prevalence rates and evidence for diminished fetal mortality and severity in genotypes associated with structural X abnormalities or mosaicism. Hum Genet 64(1):24-27. Abstract on Pubmed.
- 8. Bondy CA et al. (2007) Care of girls and women with Turner syndrome: a guideline of the Turner Syndrome Study Group. J Clin Endocrinol Metab 92(1):10-25. Full text on publisher's website.
- 9. Pasquino AM et al. (1997) Spontaneous pubertal development in Turner's syndrome. Italian Study Group for Turner's Syndrome. J Clin Endocrinol Metab 82(10):1810-1813. Full text on publisher's website.
- 10. Tarani L et al. (1998) Pregnancy in patients with Turner's syndrome: six new cases and review of literature. Gynecol Endocrinol 12(2):83-87. Abstract on Pubmed. Full text on ResearchGate.
- 11. Gunther DF & Sybert VP (2006) Lymphatic, tooth and skin manifestations in Turner syndrome. Int Congr Ser 1298:58-62. Full text.
- 12. Ford CE et al. (1959) A sex-chromosome anomaly in a case of gonadal dysgenesis (Turner's syndrome). Lancet 1(7075):711-713. Reference on PubMed.
- 13. Bernard V et al. (2016) Spontaneous fertility and pregnancy outcomes amongst 480 women with Turner syndrome. Hum Reprod 31(4):782-788. Abstract on Pubmed.
- 14. Bondy C (2014) Recent developments in diagnosis and care for girls in Turner syndrome. Adv Endocrinol 2014: Article ID 231089 doi: https://www.hindawi.com/journals/aen/2014/231089/ Full text.
- 15. Lowenstein EJ et al. (2004) Turner's syndrome in dermatology. J Am Acad Dermatol 50(5):767-776. Abstract on PubMed.
- 16. Segal D & Paediatric and Adolescent Endocrine and Diabetes Society of South Africa (2009) Guideline for using growth hormone in paediatric patients in South Africa: treatment of growth hormone deficiency and other growth disorders. S Afr Med J 99(3 Pt 2):187-195. Abstract on Pubmed. Full text from Scielo.
- 17. Photo found at Turner syndrome pictures.com (site may not load).
- 18. Bolzer A et al. (2005) Three-dimensional maps of all chromosomes in human male fibroblast nuclei and prometaphase rosettes. PLoS Biol 3(5)):e157. doi: 10.1371/journal.pbio.0030157. Full text on PubMed.
- 19. Atton G et al. (2015) The lymphatic phenotype in Turner syndrome: an evaluation of nineteen patients and literature review. Eur J Hum Genet 23(12):1634-1639. Full text on PubMed.
- 20. Photo found in the Wikimedia Commons (no author named).