Tangier Disease (TD)
Tangier disease (TD) is an inherited condition that affects the body's ability to regulate the transport cholesterols out of cells. People with TD have trouble transporting "bad" types of cholesterol out of their cells and do not have enough of the "good" types of cholesterol --- especialy a type of cholesterol called HDL cholesterol. HDL cholesterol is called good cholesterold because it removes fat molecules from artery walls, which prevents a condition called hardening of the arteries/atherosclerosis (buildup of fatty deposits on the artery walls). People who have very low levels of HDL cholesterol are at increased risk for heart disease.
TD is named for an Tangier island, a small island off the coast of Virginia. The disease was first discovered in a family there 1961 (1). Although it is a very rare disease, it may be underdiagnosed andtherefore more common than it appears to be at this time. TD has been diagnosed in many ethnic groups around the world. Unfortunately, there are no exact figures for its prevalence.
Clinical information
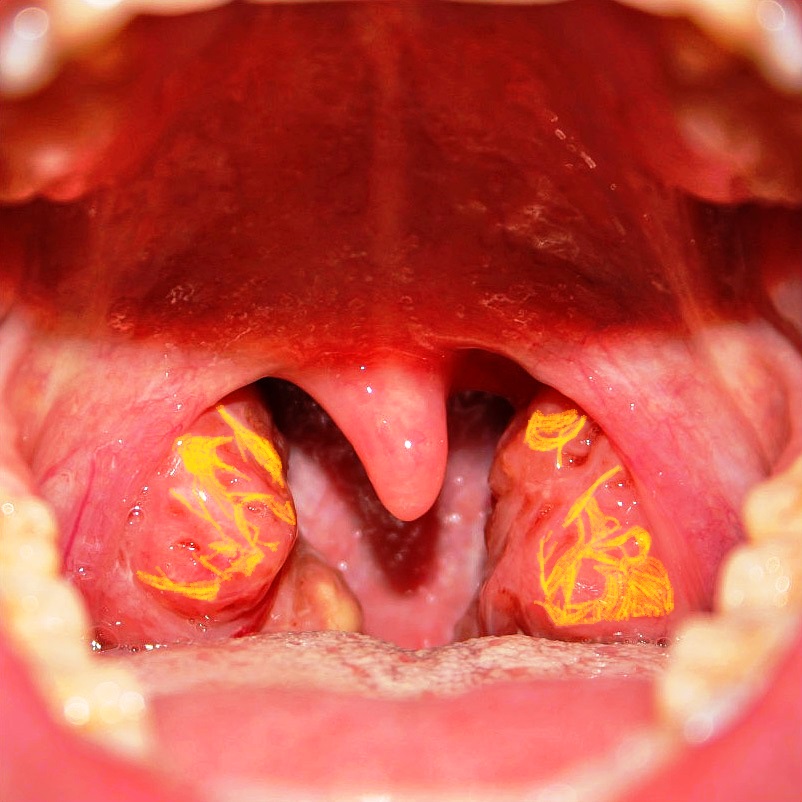
TD affects many different body systems. Its most characteristic feature is on the tonsils, where deposits of cholesterol cause them to be yellowish or orange. The photo on this page is an artist's rendition of the effect of TD on the tonsils. A patient photo is visible here. People with TD often suffer from tonsillitis, which may interfere with swallowing food. Many patients undergo tonsillectomy. Even so, yellow or orange material is often visible in the backs of the throats of patients who have had tonsillectomies. Young children may also have yellow/orange patches on the adenoids, which are small glands that sit at the back of the nasal cavity. These glands are part of the immune system and they disappear by the teenage years.
TD commonly affects the cardiovascular system and certain internal organs. In particular, an enlarged liver and/or spleen is common in TD. Roughly half of patients have cardiac abnormalities. Finally, the eyes and neurological system may also be affected. Common features of TD are listed below.
- Yellowish/orange tonsils that may frequently become enlarged
- Very low serum levels of HDL cholesterol
- Very low levels of apolipoprotein A1
- Elevated levels of triglycerides
- Cloudiness of the cornea
- Low platelet count
- Enlarged spleen
- Enlarged liver
- Chest pains
- Atherosclerosis
Common clinical features of Tangier disease
Note that while many patients with TD have elevated levels of triglycerides in their blood, levels may be normal in some.
Signs of TD may not be obvious at birth or in childhood. However, any child with yellow/orange tonsils should be checked for TD and monitored carefully for abnormalities in the blood.
Neurological problems in Tangier disease
In addition to the problems noted above, roughly half of people with TD also develop neurological problems. Their specific problems tend to be among the clinical features in the list below, and tend to fit the definition of a condition called polyneuropathy. This term refers to disease that affects the peripheral nerves. Common problems include weakness, numbness, and burning pain. However, the way that these problems occur varies, especially in TD.
A 1985 study proposed that there are 3 subtypes of polyneuropathy in TD (2). We have not found any publications that have updated this information and present it here as a guide.
Type I TD polyneuropathy is transient or relapsing. These term means that the symptoms like weakness may come and go, and may not last for long periods when they occur. The symptoms are asymmetrical, meaning that they may only occur on one side of the body. In addition, a process called nerve conduction velocity (NCV) is usually, but not always, normal in Type I TD neuropathy. NCV is a measure of how quickly nerve transmit impulses. Patients with this form of TD polyneuropathy are described in references 3 and 4.
Type II TD polyneuropathy is a slowly progressing form. Thus, once problems begin, they do not tend to go away for a while, and they continue to get worse as time passes. Unlike type I, in type II, problems occur on both sides of the body. These problems are most marked in the lower extremities, and like type I, nerve conduction velocity is normal. A patient with this form of TD is described in reference 3.
Type III TD polyneuropathy is also a slowly progressing symmetrical condition. Unlike type II, atrophy and weakeness tend to occur in the upper extremities (especially in the distal parts, or hands and other parts of the arms that are furthest from the shoulders). Nerve conduction velocity is not normal in type III TD polyneuropathy and is slower or much slower than normal. A patient with this condition is described in reference 2.
Patients with all three neurological forms of TD may lose the sensations of pain and temperature. This problem makes them susceptible to burns, which may occur without their knoweldge until damage has been done.
- Peripheral neuropathy (weakness, numbness, pain, usually in hands and feet)
- Abnormal results of test of motor nerve conduction velocity
- Muscle weakness (may get worse or relapse and remit)
- Lost/reduced deep tendon reflexes (e.g. knee jerks)
- Myelin abnormalities in peripheral nerves
- Reduced temperature sensitivity
- Reduced pain sensitivity
- Muscle wasting
Neurological features of Tangier disease
Cause and disease manifestations in carriers
Tangier disease is caused by mutations in a gene called ABCA1. This gene encodes a protein that moves cholesterol and other lipids out of cells. When ABCA1 is mutated, these substances accumulate in cells,with the result that some of them swell and turn yellowish-orange color. Heart disease and hardening of arteries are also a common result of mutations in ABCA1.
TD is an autosomal recessive disorder. The term autosomal recessive means that the disorder is passed on when both parents contribute a copy of the mutated gene to their child.
People with one copy of a mutated gene and one normal one are called carriers. Carriers of autosomal recessive diseases do not usually have signs of the disease themselves, but this is not the case in TD. Rather, TD carriers have low levels of HDL cholesterol and increased levels of triglycerides (5-7). They also have an increased risk of developing heart disease (5, 8). Thus, it is important to monitor the heart health of carriers of TD. This group includes not only parents of patients, but potentially siblings as members of the extended family as well. Ideally, family members should be tested for mutations in ABCA1.
Diagnosis
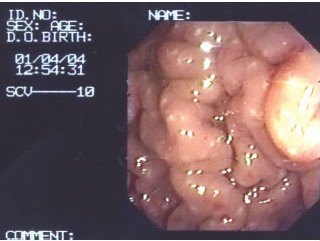
A key finding in Tangier disease is yellowish-orange tonsils that may often become swollen. Frequent swelling often leads to a tonsillectomy; however, even in this case, yellow/orange patches may still be visilble in the pharynx (rear of the upper throat). These abnormalities are present in a large majority of patients. In addition, the rectal mucosa and/or the stomach lining may also have yellowish areas that are essentially composed of lipid deposits.
All TD patients have very low levels of HDL cholesterol and very low levels of apolipoprotein A1. These findings are often combined with normal or elevated levels of triglycerides and overall low levels of total cholesterol. Some patients also have neurological problems as described above. Diagnosis can be confirmed with genetic testing. Clicking the link at the right will provide information on labs that test for TD.
Note that there are other conditions that cause very levels of HDL cholesterols (see Differential Diagnosis, below).
Differential Diagnosis
Familial LCAT deficiency. LCAT stands for lecithin cholesterol acyltransferase. LCAT is an enzyme that is involved in removing cholesterol from the blood and tissues. Thus, it does a job similar to ABCA1, which is mutated in TD. Not surprisingly, TD and LCAT deficiency share many clinical features, including low levels of HDL cholesterol, cloudiness of the cornea, enlargement of the liver and/or spleen, and hardening of the arteries. One important difference between them is that LCAT patients have serious problems with kidney disease, while TD patients do not. Seaquencing of the genes ABCA1 and LCAT can distinguish the two conditions. Another form of LCAT deficiency is called fish-eye disease; it has this name because cloudiness of the cornea is a prominent feature. This form of LCAT deficiency is less severe than the familial form.
Apolipoprotein A-I deficiency (AA1D). The clinical features of AA1D are also similar to those of TD: low HDL cholesterol, normal or increased levels of triglycerides, clouding of the cornea, and increased risk of heart disease. AA1D patients may have no or barely detectable levels of apolipoprotein A1 in their blood plasma. Although the number of cases reported to date is very low, people with this condition do not appear to have abnormalities of the tonsils (especially orange/yellow discoloration). AA1D is caused by mutations in the gene APOA1, and gene sequencing can distinguish it from TD.
Steroid use or abuse. Use of anabolic-androgenic steroids can lower HDL levels and increase the risk of heart disease. Compounds that have this effect include testosterone and/or its synthetic derivatives, such as nandrolone decanoate (Deca Durabolin or Deca), methandienone (Averbol, Dianabol, Danabol, Metanabol, Naposim, Vetanabol), stanozolol (Winstrol or Winny), androsterone, and androstane. In addition to low levels of HDL, steroids may also induce atrophy of the testicles, growth of breast tissue in males, and psychiatric problems (9). These features may help distinguish the two conditions. In addition, a finding of a mutation in ABCA1 can diagnose TD.
Charcot-Marie-Tooth Disease (CMT). CMT is actually a group of diseases that affect motor nerves and sensory nerves. Overall, CMT is characterized by muscle weakness, muscle atrophy, and loss of sensation, such as loss of pain sensation and loss of sensitivity to heat. All of the TD neurological symptoms listed in the table above also occur in CMT. However, low HDL cholesterol and yellow-orange patches on the tonsils or throat are not features of CMT, and the two can be distinguished that way.
Hansen's disease (leprosy). The neurological problems that occur in TD can resemble problems that happen in people with leprosy. They include weakness, muscle atrophy/wasting, peripheral neuropathy, and loss of sensation. Leprosy may cause clouding of the cornea. Extremely low levels of HDLs are not associated with leprosy, but high HDL levels are known to occur in lepromatous leprosy (10). Certain other features of leprosy are not generally seen in TD. They include a variety of skin lesions that may lose their pigmentation (see our leprosy page for photos), loss of digits, and thickening of large nerves (the nerve may stand out under the skin. Laboratory testing can distinguish the two conditions.
Obviously, this particular differential diagnosis is most important in people who come from regions where leprosy is common, or who have spent considerable time in one or more of these places.
References
- 1. Fredrickson DS et al. (1961) Tangier disease: combined clinical staff conference at the National Institutes of Health. Ann Intern Med 55(6):1016-1031. Publisher website.
- 2. Gibbels E et al. (1985) Severe polyneuropathy in Tangier disease mimicking syringomyelia or leprosy. Clinical, biochemical, electrophysiological, and morphological evaluation, including electron microscopy of nerve, muscle, and skin biopsies. J Neurol 232(5):283-294. Abstract on PubMed.
- 3. Engel WK et al. (1967) Neuropathy in Tangier disease. Alpha-lipoprotein deficiency manifesting as familial recurrent neuropathy and intestinal lipid storage. Arch Neurol 17(1):1-9. Abstract on PubMed.
- 4. Pollock M et al. (1983) Peripheral neuropathy in Tangier disease. Further observations. Brain 106(Pt. 4):911-928. Abstract on PubMed.
- 5. Clee SM et al. (2000) Age and residual cholesterol efflux affect HDL cholesterol levels and coronary artery disease in ABCA1 heterozygotes. J Clin Invest 106(10):1263-1270. Full text on PubMed.
- 6. Cohen JC et al. (2004) Multiple rare alleles contribute to low plasma levels of HDL cholesterol. Science 305(5685):869-872. Full text from publisher.
- 7. Frikke-Schmidt R et al. (2004) Genetic variation in ABC transporter A1 contributes to HDL cholesterol in the general population. J Clin Invest 114(9):1343-1353. Full text on PubMed.
- 8. Schaeffer EJ et al (1980) Coronary heart disease prevalence and other clinical features in familial high-density lipoprotein deficiency (Tangier disease). Ann Intern Med 93(2):261-266. Abstract on PubMed.
- 9. Payne JR et al. (2004) Cardiac effects of anabolic steroids. Heart 90(5):473-475. Full text on PubMed.
- 10. Kumar N et al. (1988) Estimation of high density lipoprotein cholesterol in the diagnosis of lepromatous leprosy. Indian J Lepr 60(4):600-603. Abstract on PubMed.
- 11. Klem, Wikimedia Commons member (2007). Photograph of tonsils. Public domain reproduction.
- 12. National Eye Institute (2007). A TD patient with an opacity of the cornea. Wikimedia Commons. Public domain reproduction.
- 13. Espinel J et al. (2006) Gastric mucosa appearance in a patient with Tangier disease. Rev Esp Enferm Dig 98(10):786-787. Full text from Scielo.