Hashimoto's encephalopathy (HE)
Hashimoto's encephalopathy (HE) is an autoimmune condition. The term autoimmune means that a person's body mistakenly attacks itself. Rheumatoid arthritis (RA) is an example of an autoimmune disease. It attacks the linings of joints, which causes causing swelling and pain. Eventually, bone can be eroded as they scrape against one another, and joints can become deformed. There are also thyroid abnormalities. In HE, the brain is affected and patients have neurological and psychiatric problems. The cause or causes of HE are currently not known, but most patients respond to therapy with steroids.
Because of the steroid connection, HE is also called steroid-responsive encephalopathy associated with autoimmune thyroiditis, or SREAT. Another name for it is encephalopathy associated with autoimmune thyroid disease, or EAATD. However, the term Hashimoto's encephalopathy remains in popular usage, and we will use HE here.
The prevalence of HE has been estimated at 2.1 per 100,000 in Italy (1). No other prevalence estimates have been made. However, HE has been described in people from races and ethnic groups around the world. If the Italian figure applies in the United States, there are roughly 6,500 people with HE in this country. Females are far more likely to have HE than males. We analyzed 142 published case histories, and sex information was available for all of them. Exactly 80% of patients were female, with 20% male. This figure matches exactly with a previous large study of the literature (2).
Clinical information
Two broad categories of abnormalities occur in HE: encephalopathy (brain disorder) and the presence of antithyroid antibodies in the serum.
Encephalopathy. Encephalopathy in HE manifests in a variety ways. Patients may have seizures, alterations of consciousness, dementia and various cognitive problems, and/or various psychiatric problems. People may have all of these abnormalities or only a limited number of them.
HE is classified into two forms: diffuse-progressive and vasculitic. There is overlap between these two forms. In general, however, the diffuse-progressive form tends to get worse with time, while the vasculitic form tends to come and go. Thus, patients with diffuse-progressive HE tend to experience continuous deterioration of cognitive functions that gets worse with time. They may become confused and disoriented with respect to time and place, and suffer from memory loss. They may also have hallucinations and suffer from psychosis. Those with the vasculitic form suffer from stroke-like episodes that tend to come and go. Such episodes may include headaches, drowsiness, apathy, and focal neurological deficits (e.g. weakness, paralysis, speech difficulties, and abnormal sensations). Seizures occur in both groups, and in spite of the two classifications, problems may relapse and remit or be steadily progressive in a single person.
Antithyroid antibodies. To date, all patients with HE have had elevated serum levels of antithyroid antibodies (anti-thyroid peroxidase antibody [anti-TPOAb], anti-thyroglobulin antibody [anti-TgAb], and/or anti-microsomal antibodies). The role of these antibodies in the disease process is not currently known, and serum antibody levels do not correlate with severity or stage of disease (3-5). In addition, elevated antithyroid antibodies occur in patients with other disorders (1) and occur in up to 10% of the normal population (6, 7). Serum levels of these antibodies may increase with advancing age, especially in women (8). There is also no evidence showing that antithyroid antibodies react with brain tissue or affect the functon of nerves, making the universal presence of these antibodies in HE patients a mystery.
HE is often associated with Hashimoto's thyroiditis (HT), although patients with HT will not necessarily develop HE. HT is also known as Hashitmoto's disease. Like HE, HT is an autoimmune disorder that affects the thyroid gland. People with HT have hypothyroidism (an underactive thyroid gland). The symptoms of this condition are generally different from those of HT: they include fatigue, cold sensitivity, a puffy face, weight gain, and dry skin. Although HT patients may experience weakness and depression, the severe neurological and psychiatric symptoms that occur in HE are not a feature of Hashimoto's thyroiditis. In addition, not all patients with HE have a history of hypothyroidism. Our analysis found hypothyroidism in only 62% of patients, with some having had the problem in the past, but not at the time of symptom onset.
Some people with HE have a history of Graves disease, which causes hyperthyroidism. Again, having Graves disease does not mean that Hashimoto's encpehalopathy will develop, and the connections between the two conditions are not understood.
People with HE can experience a variety of different problems. The following are common clinical features in HE (this list is not exhaustive):
- Seizures
- Myoclonus
- Memory loss
- Encephalopathy
- Hallucinations
- Behavior change
- Personality change
- Speech abnormalities
- Loss of cognitive abilities
- Disorientation or confusion
- Change in level of consciousness
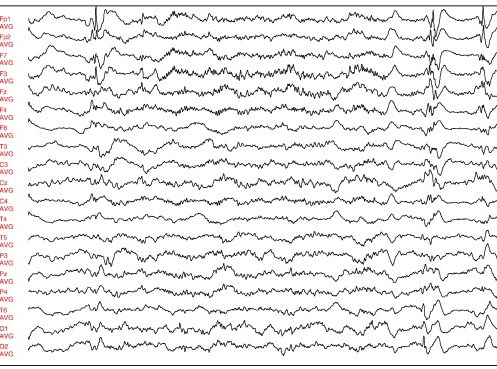
- EEG abnormalities (see figures on this page)
Common clinical features of Hashomoto's encephalopathy
Other signs and symptoms include weakness on one side of the body, headache, vertigo, and tremors. As noted, these problems may come and go, or they may have a sudden onset and be progressive. In addition, HE may present as a medical emergency or as a series of episodes of problems that resolve and reappear with time.
Diagnosis and Testing
HE is suspected in a person with two broad findings: 1) encephalopathy that is either relapsing/remitting or progressive, combined with 2) high levels of antithyroid antibodies in the serum. Raised levels of antithyroid antibodies are essential for diagnosis, but do not cornfirm it (2). There is currently no general consensus regarding exact diagnostic criteria for HE, but there is consensus that the two features noted above are present in all people with HE. There are also no specific laboratory tests that can definitively diagnose HE.
Laboratory and other tests can help point toward a diagnosis of HE. One important test is electroencephalography (EEG). EEG findings in HE are often abnormal, though there are no specific abnormalities associated with HE. The most frequently reported problem is background slowing (generally in the delta range). In our analysis of published cases, EEG data was available for 133 patients, and abnormal readings were found in 113 (89%). Oddly, in spite of the fact that seizures are common in HE (>60% of cases we analyzed), epileptiform discharges are rarely seen in EEGs of people with HE. Periodic triphasic spikes do not appear to be a feature of the EEG in HE. These spikes are characteristic of Creutzfeldt-Jakob disease (CJD; 2). See the section entitled Differential Diagnosis for more information on CJD and HE.
CSF analysis is also important. In our review, information on CSF analysis was available for 135 patients; total CSF protein was elevated in nearly 2/3 of this group. Antithyroid antibodies may also be found in the CSF (16 out of 26 CSF samples tested in one study were positive).
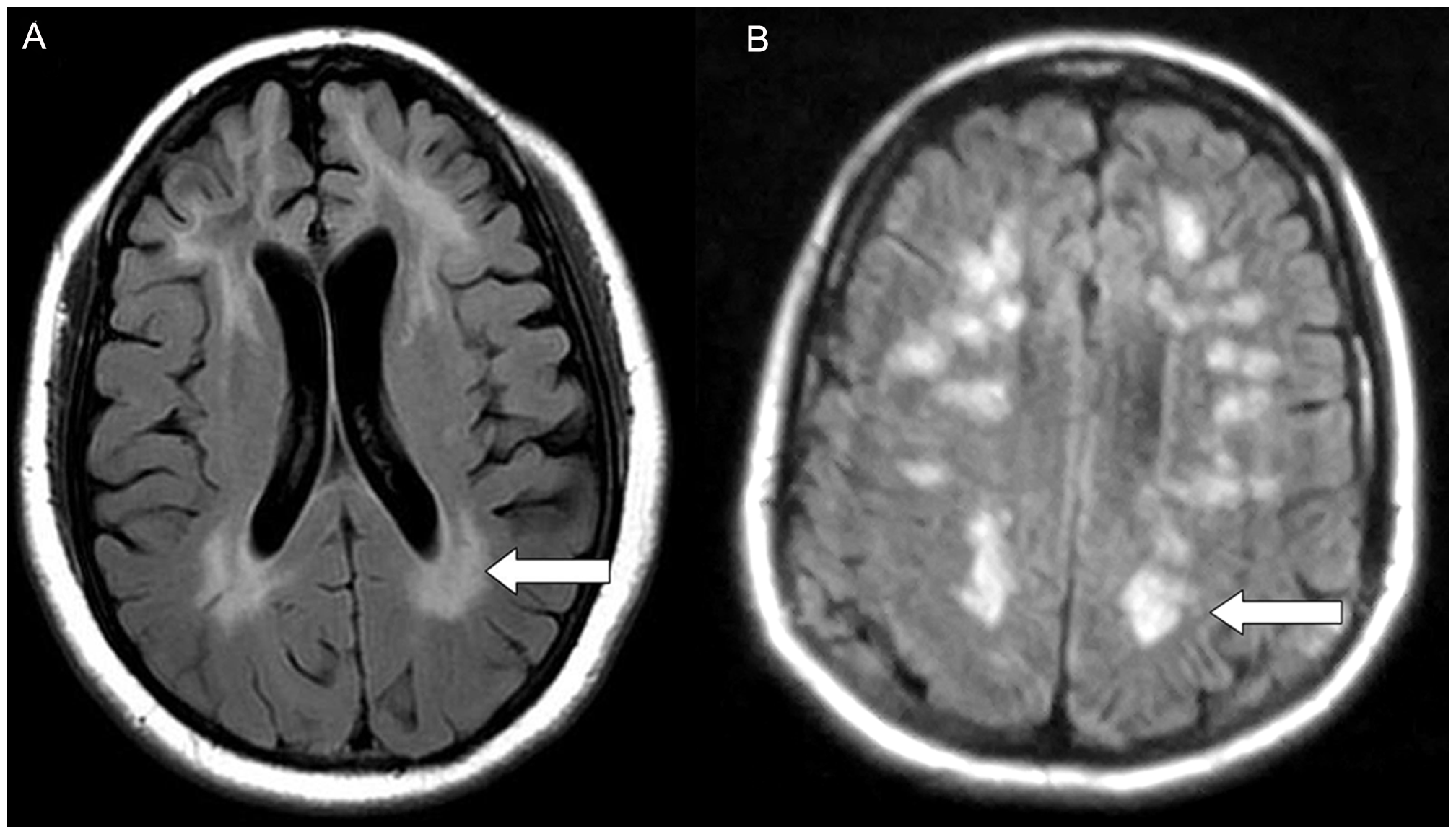
MRI has also been performed on people with HE. As with EEG readings, there are no specific abnormalities that identify HE. The most common findings are white matter abnormalities, cerebral atrophy, and cerebellar or white matter hyperintensities (2). Imaging studies were reported in just over 100 patients in the published case histories we analyzed. White matter abnormalities were noted in 29% of them, and brain atrophy in 17%.
HE is often called a diagnosis of exclusion. This term means that a variety of other conditions should be excluded before diagnosing HE. Conditions that are similar to HE include CJD and Alzheimer's disease (AD). Other conditions to exclude include infectious encephalopathies, vitamin deficiencies and metabolic disorders such as Wilson's disease, and various dementias. See Differential Diagnosis below for a discussion of these conditions and HE.
It should be noted that because HE often responds to treatment, while conditions like CJD and AD do not, it is likely a good idea to check for elevated antithyroid antibodies in any patient suspected of having CJD or another disorder in the differential diagnosis for HE. Of note in this regard, one study of patients diagnosed with CJD found 7 who were found to actually have HE (9). All seven patients recovered after being treated with steroids. Suspicion or diagnosis of CJD in people who were later diagnosed with HE has been reported elsewhere (10, 11). Two patients were diagnosed after death (11).
Many patients with HE have a history of thyroid abnormalities (hyper- or hypothyroidism), but some have normal thyroid function. Some have a history of Hashimoto's thyroiditis or Graves disease (another autoimmune condition affecting the thyroid), but some do not. For example, in a large review of 121 people with HE, 32 had a history of Hashimoto's thyroiditis, 3 had a history of Graves disease, and 2 had a goitre (2). This left 84 patients without a history of thyroid disease.
Differential Diagnosis
The differential diagnosis of HE includes a number of other conditions, including Creutzfeldt-Jakob disease (CJD), Alzheimer's disease, various microbial encephalopathies, and other dementias.
Creutzfeldt-Jakob disease (CJD). CJD and HE can look very similar. Both feature dementia, personality change or psychosis, myoclonus, and ataxia as characteristic symptoms. In addition, CJD is a progressive disorder, as is the case in a majority of HE patients. As a result, they can be almost indistinguishable. A lab test for 14-3-3 protein in the CSF can help distinguish the two. This protein is not generally present in the CSF of HE patients, although isolated reports have found it (12-14), CSF has not been found in the CSF of any other patients when it was sought (9, 13, 16, 17). False positives for 14-3-3 can occur after seizures, infection, inflammation, and ischemia.
EEG may also be useful in distinguishing CJD from HE. Like HE patients, CJD patients in the early stages may show diffuse slow waves on EEG. However, as CJD progresses, biphasic and triphasic periodic sharp wave complexes are often observed (see here for an example). These waves have not been reported in HE (2), although they do occur in SSPE, a neurological complication of measles virus infection.
CJD is an extremely rare disease, with estimates for its annual incidence at 1.67 per million for all cases and 1.39 per million for sporadic cases (15). Sporadic cases comprise a large majority (85-90%) of all CJD cases. In addition, sporadic CJD is rapidly fatal, with death occuring within a year of diagnosis, implying that prevalence and annual incidence may be roughly equal. Comparing the HE prevalence estimate of 2.1 per 100,000 and the CJD figure implies that HE may be roughly 15 times as common as CJD. The implication is that any patient suspected of having untreatable, fatal CJD should be tested for serum antithyroid antibodies to rule out treatable HE.
Alzheimer's disease (AD). AD is a common form of dementia, affecting 1 person in 9 over age 65 (more than 5 million Americans). People with AD have trouble with retaining memories of recent events, such as conversations or occurences. They may forget to turn a burner off or forget a neighbor's name. They may also become easily disoriented, even in familiar places, or be unable to follow directions. Other signs of AD include speech difficulties, personality and behavior changes, hallucinations, and agitation. Some of these abnormalties, such as executive dysfunction and dementia, are also associated with FXTAS, especially in its later stages (18).
While distinguishing AD and HE may be difficult, some factors may help. For example, seizures are uncommon in AD, but are common in HE (epileptic seizures were reported in 61% of the patients in our literature review). Weakness occurs in as many as half of HE patients, but is relatively uncommon in AD, and appears to be a late-stage abnormality in AD. Weakness is, however, a feature of other forms of dementia.
Encephalopathies caused by microorganisms. A variety of infectious organisms can cause encephalopathies. They include HIV, hepatitis viruses, and various bacteria. Although infectious encephalopathies can resemble HE, eliminating them from diagnostic consideration is possible through testing for them in CSF or serum. Such testing should be done as a matter of course in an person suspected of having HE or another condition that causes dementia.
Other conditions in the differential diagnosis for HE include metabolic encephalopathies and other forms of dementia, such as Wilson's disease and Pick's disease.
Overall, the clinical and laboratory features of HE are very similar to those of CJD, AD, and other forms of dementia. This fact makes distinguishing them difficult. Testing for antithyroid antibodies is suggestive of HE, but given that up to 10% of the population has elevated serum levels of these antibodies, their presence does not rule out AD, CJD, and the other conditions noted above. In some cases, response to treatment with steroids may be a route to diagnosis. Clearly, the decision to treat must be made by an experienced clinician who is aware of a patient's overall health status.
The links at the right will provide a list of clinical trials for HE and Hashimoto's thyroiditis. At the time this page was written, no trials for HE were found. However, if any become listed in the clinicaltrials.gov database, they should appear when the link is clicked.
Treatment
HE is generally a treatable condition. Corticosteroids are the most commonly used first line of treatment, although a variety of other options have also been used (2). One summary of therapies given in HE found that of 91 patients treated with corticosteroids alone, 87 showed some kind of improvement. Forty-two had stable improvement, 34 had temporary improvements but suffered relapses, and 11 improved but some deficits remained (2). Corticosteroids in combination with other agents have also been used. The other agents include L-thyroxine, azathioprine, cyclophoshamide, and phenytoin. Of 19 patients treated with combinations of these drugs, 14 had stable improvement, 2 improved with residual deficits, 2 improved but had relapses, and 1 did not improve.
Other therapeutic agents have included L-thyroxine alone or incombination with valproate, plasma exchange, plasmapheresis (also called plasma exchange), intravenous immunoglobulin (IVIG), azathioprine plus methotrexate, carbimazole, and flunarizine (2). L-thyroxine was used in 10 patients with stable improvement in 4, and the others were used in less than 5 patients each.
In many studies, clinical improvement treatment correlates with improvements on EEG and MRI (see references 3 and 19 for examples). Unfortunately, to date, there have been no controlled studies of therapies for HE. In addition, the treatments that have been used to date used different protocols. These facts mean that it is not possible to perform a statistical analysis on treatment information in the literature, nor is it possible to rate the effects of the different drugs that have been used in HE.
References
- 1. Ferracci F et al. (2004) Hashimoto's encephalopathy: epidemiologic data and pathogenetic considerations. J Neurol Sci 217(2):165-168. Abstract on PubMed.
- 2. Ferracci F & Carenvale A (2006) The neurological disorder associated with thyroid autoimmunity. J Neurol 253(8):975-984. Abstract on PubMed.
- 3. Castillo P et al. (2006) Steroid-responsive encephalopathy associated with autoimmune thyroiditis. Arch Neurol 63(2):197-202. Full text from publisher.
- 4. Chong JY et al. (2003) Hashimoto encephalopathy: syndrome or myth? Arch Neurol 60(2):164-171. Full text from publisher.
- 5. Olmez I et al. (2013) Diagnostic and therapeutic aspects of Hashimoto's encephalopathy. J Neurol Sci 331(1-2):67-71. Abstract on PubMed. Full text on ResearchGate
- 6. Flynn SD et al. (1988) Autoimmune thyroid disease: immunological, pathological and clinical aspects. Clin Lab Sci 26(1):43-95. Abstract on PubMed.
- 7. Yoneda M et al. (2007) High prevalence of serum autoantibodies against the amino terminal of alpha-enolase in Hashimoto's encephalopathy. J Neuroimmunol 185(1-2):195-200. Abstract on PubMed.
- 8. Roti E et al. (1992) Prevalence of anti-thyroid peroxidase antibodies in serum in the elderly: comparison with other tests for anti-thyroid antibodies. Clin Chem 38(1):88-92. Full text from publisher.
- 9. Seipelt M et al. (1999) Hashimoto's encephalitis as a differential diagnosis of Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry 66(2):172-176. Full text on PubMed.
- 10. Doherty CP et al. (2002). Hashimoto's encephalopathy mimicking Creutzfeldt-Jakob disease: brain biopsy findings. J Neurol Neurosurg Psychiatry 73(5):601-602. Full text on PubMed.
- 11. Poser S et al. (1999) How to improve the clinical diagnosis of Creutzfeldt-Jakob disease. Brain 122(Pt 12):2345-2351. Full text from publisher.
- 12. Creutzfeldt CJ & Haberl Rl (2005) Hashimoto encephalopathy: a do-not-miss in the differential diagnosis of dementia. J Neurol 252:1285-1287. Abstract on PubMed.
- 13. Hernàndez Echebarrià LE et al. (2000) Detection of 14-3-3 protein in the CSF of a patients with Hashimoto's encephalopathy. Neurology 54:1539-1540. Abstract on PubMed.
- 14. Vander T et al. (2004) Detection of 14-3-3 protein in the CSF of a patients with Hashimoto's encephalopathy. J Neurol 251(10):1273-1274. No abstract available.
- 15. Ladogana A et al. (2005) Mortality from Creutzfeldt-Jakob disease and related disorders in Europe, Australia, and Canada. Neurology 64(9):1586-1591. Abstract on PubMed.
- 16. Spiegel J et al. (2004) Progressive dementia caused by Hashimoto's encephalopathy-report of two cases. Eur J Neurol 11(10):711-713. Abstract on PubMed.
- 17. Cao NJ et al. (2005) A case of Hashimoto's encephalopathy: association with sensory ganglionopathy. J Neurol Sci 238(1-2):105-107. Abstract on PubMed.
- 18. Wang J et al. (2013) Cognitive impairments in Hashimoto's encephalopathy: a case-control study. PLoS One 8(2):e55758. Full text on PubMed.
- 19. de Cerqueira AC et al. (2008) Hashimoto's encephalopathy with clinical features similar to those of Creutzfeldt-Jakob disease. Arq Neuropsiquiatr 66(4):903-905. Full text from Scielo.
- 20. Visée H et al. (2013). Recurrent status epilepticus associated with Hashimoto's encephalopathy. Epilepsy Behav Case Rep 15(1):113-117. Full text on PubMed.
- 21. Kang WH et al. (2013) Hashimoto's Encephalopathy Presenting with Acute Cognitive Dysfunction and Convulsion J Epilepsy Res 3(2):70-73. Full text on PubMed.